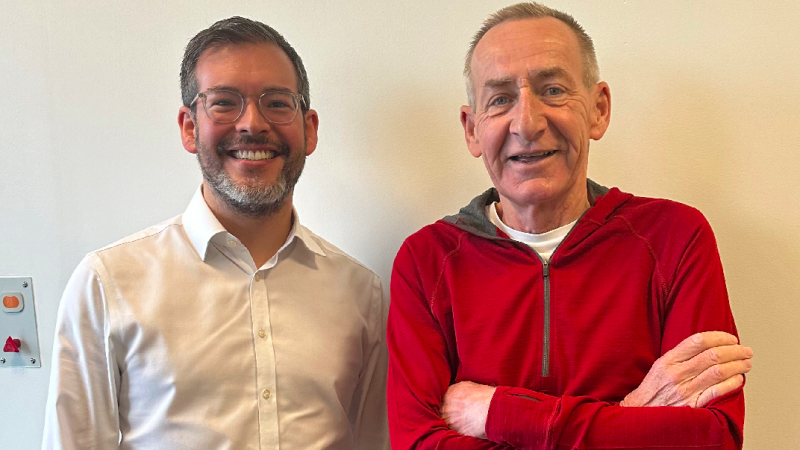
*Photograph – Patient Morgan Wallace with oncology consultant Dan Lee.
The introduction of remote monitoring virtual wards at Leeds Teaching Hospitals NHS Trust is helping patients to return home sooner and reducing their average length of stay by five days, according to estimates of the first six months of the service.
Launched in partnership with Inhealthcare, the virtual wards provide an alternative to admission or enable earlier discharge for patients requiring daily monitoring but stable enough to be in their usual residence.
As a result, the trust saved an estimated 959 bed days between November and April with an estimated efficiency saving of £372,000, equivalent to nearly £15,000 per week. A total of 176 patients used the service during the period.
The first six pathways are within abdominal medicine and surgery and oncology. The trust plans to expand the service to add six more pathways for patients with vascular, neurological and pancreatic conditions, with further additions to follow in the future.
Leeds is one of the largest NHS trusts in the UK with 2,050 beds and last year made nearly 94,000 inpatient admissions.
Abigail Uttley, service manager at Leeds Teaching Hospitals NHS Trust, said: “While developing a service that is directly assisting the NHS with the crisis of over-occupied beds, it has been rewarding to see our remote monitoring virtual wards come to life, enabling patients to be cared for in their own homes with the safety of technology.
“Remote monitoring is the most effective way in ensuring patients can be discharged safely but still receive excellent care.”
‘Remote monitoring virtual wards a game-changer for managing patients’
Adam Peckham-Cooper, lead consultant for emergency general surgery, added: “The remote monitoring virtual wards have been a game-changer for expeditiously managing patients in a different way safely and effectively.
“We have for many years held on to a varied set of patients in hospital beds awaiting investigations, interventions or just for ongoing observation. By using the bespoke pathways, we have managed to facilitate earlier discharges and streamline ambulatory care of patients, vastly improving patient experiences.”
Patient feedback has been positive with surveys showing the vast majority of respondents found the service easy to use, felt comfortable being monitored and spoke with clinicians when they needed to. Respondents added the virtual wards saved travel time to and from hospital and improved their health care experience.
One of the first patients to use the service was Toni Bailey, a 28-year-old mother of two young children from Leeds who was admitted to hospital after Christmas with severe abdominal pain. After two weeks in hospital undergoing treatment for pancreatitis, she was able to join the virtual ward.Toni said: “Home is the best hospital in the world. I was desperate to get home to my family. It meant I could be in my own bed, eat my own food and be with my children to lift my spirits while being closely monitored by a brilliant team of nurses. If I hadn’t had the opportunity to join the virtual ward, I believe I would have been ill a lot longer.”
Morgan Wallace, a 66-year-old retired headteacher from Otley in West Yorkshire, was diagnosed with lung cancer last year. As part of his treatment involving chemotherapy and immunotherapy, he experienced infections that required hospital stays for IV antibiotics. During his last infection, doctors suggested Morgan try the virtual ward to recover at home.
Morgan said: “If you’ve got the opportunity, if it means getting out of the hospital and getting home, I would jump at the chance. Nobody likes to be in a hospital. You’re obviously much better when you’re at home.”
‘The safest level of care’
The trust has established a multi-specialist nursing team which works with lead clinicians to make sure they provide the safest level of care to patients.
Alessia D’Angelo, senior sister for remote monitoring virtual wards, said: “The technology is used extremely well in care pathways, offering patients reassurance at home, where anxiety may arise, particularly before procedures. It proves invaluable during hospital admissions, providing recent observations to aid decision-making.
“Remote monitoring provides a crucial safety net when in-person appointments are unfeasible, enabling patients to share recent health readings for informed care decisions outside normal hours.”
Patients or their caregivers are empowered to take physiological measurements such as blood pressure, respiration rate and oxygen saturation and securely transmit their readings to care teams via a choice of digitally inclusive communication channels – mobile app, text message or traditional telephone. Care teams have a single, centralised view of patient data to support clinical decision making and if any readings fall out of range, they are alerted to enable early intervention.
Muzahir Tayebjee, lead consultant for the programme, said: “The use of remote monitoring equipment in conjunction with the virtual ward increases the safety and efficiency of the service, while also reducing the workload on ward staff by eliminating the need for them to take time to record these observations.”
Bryn Sage, chief executive of Inhealthcare, said: “Our technology aims to reduce admissions, speed up discharge and ease pressure on hospital beds and emergency departments.”
Natalie Duffield, sales and marketing director of Inhealthcare, added: “As a Yorkshire company, we are delighted to be working with Leeds Teaching Hospitals NHS Trust and helping to improve patient experience and deliver personalised care.”
Following a central West Yorkshire procurement, Inhealthcare won the NHS contract to develop and expand virtual wards across Calderdale, Kirklees, Leeds, and Wakefield to support the delivery of safe and convenient care to people at home who would otherwise be in hospital.
Read the full case study here.